Where do broken hearts go? A midnight reflection on mental health and mental health services within hospitals.
Patient in a hospital bed.
Everywhere you turn, you are reminded that we are living in unusual times, with words like “unprecedented” banded around often. We are also reminded of self care and mental well-being due to the effects of the pandemic and lock-down changing our way of lives for the foreseeable future if not forever- whats being called “the new normal”.
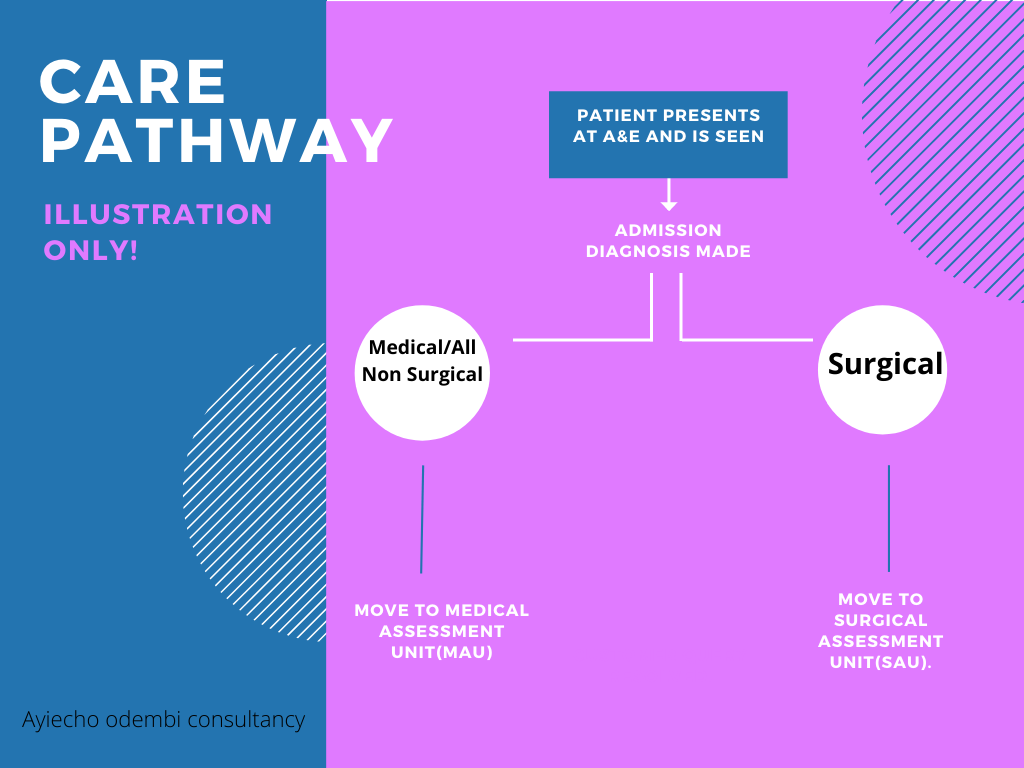
So there i was in the middle of the night, sleep having escaped me and Whitney Houston’s song ‘where do broken hearts go?’ playing over and over in my head, wondering where patients who presented with mental health problems went after coming into A&E? Or why , in my all my years in nursing, the only times i came across a mental health nurse was at university and when a psych consult was ordered on the unit/ward. Typically, when patients presented in A&E, and need admission, there are two routes normally followed- admission to the Medical assessment unit(MAU) or to the Surgical assessment unit(SAU). Most mental health patients end up in MAU or poisons unit( if admitted due to overdose and where such a unit is available and has empty beds).
Most of the time i have been involved in looking after a patient with mental health issues, it has been on an acute medical ward. This has been usually in the bays closest to the nurses patients reserved for patients who are acutely ill and need constant nursing supervision, which often involves bright lights, regular vital sign monitoring and other checks as per care plan with a hive of activity going on around due to the nature of varying acutely ill patients around. This got me wondering if an acute medical ward really is the right setting for someone going through a mental health crisis, given that they are being looked after by nurses, not mental health nurses, who yes might be doing a brilliant job and are good at what they do but are not aware of triggers or care pathways for someone going through a mental health crisis as a trained mental health nurse would with the patient in the right setting.
With a little help………
According to Mind¹, a leading mental health charity, mental health problems are common in England with 1 in 4 people experiencing some sort of mental health problem each year and 1 in 6 reporting having experienced a common mental health problem like anxiety or depression in any given week.
A study by The Nuffield Trust² looking at hospital use by people with mental health illness, makes for an interesting and sober reading and highlights a number of key points that need addressing. With almost every NHS hospital trust having a Medical assessment unit or a Surgical one, maybe it is time there was also a Mental health assessment unit where those coming into hospital with a mental health illness can get the care they deserve, looked after by trained mental health staff under conducive conditions designed with them in mind. I would certainly welcome a unit like that, where me and my fellow healthcare workers can pop into just for a chat or to make sense of life and all its challenges especially after a hard and emotionally draining day at work given the pressures we are constantly under with the added effect that this pandemic adds to it and i would be happy to know that mental health just like physical health, matters and that those going through any sort of mental health illness can come into hospital knowing that they have a dedicated area that’s ready to to help them in anyway possible.
Dr. Chisholm - the first Director-General of the World Health Organisation (WHO)
The NHS is returning to ‘normal’. Backlog and patient safety
Putting patientsafety at the front ,back and center of every decision as the NHS tries to deal with the huge backlog of cases as it tries to return to 'normal' #effectsofcovid19 #patientcare #covid19uk #healthcare
Click on the link below to read a brilliant piece by Patient Safety Learning on concerns about patient safety and the backlog of cases that face the NHS as it tries to return to normal post Covid-19
Telemedicine in Kenya - 5 years on!
Telemedicine was meant to revolutionise primary health care delivery in Kenya. Five years on, has it?
Technology can play an important part in healthcare, as is currently evident in the role it has played in the fight against Covid-19. Indeed early this year in March, Kenyatta National Hospital (KNH), launched a telemedicine technology center for the detection of Coronavirus, touted as the first of its kind in Africa. Telemedicine allows healthcare professionals to evaluate, diagnose and treat patients at a distance using telecommunications technology.
A quick google search on telemedicine in Kenya, shows that its not a new concept in Kenya. In fact 2015 saw the launch of two telemedicine schemes, that were meant to revolutionise healthcare delivery to Kenya’s rural poor and marginalised communities. The first scheme was a collaborative venture between German based Merck group and the Ministry of Health, that provided a platform which enabled both patients and healthcare providers in rural areas to interact with Kenyatta National Hospital health experts via video conferencing. The second scheme, Sema-Doc was launched by the First Lady Margaret Kenyatta and for monthly fee of 300 Kenyan shillings you would get access to medical doctor plus a whole range of other services by dialing *220# on ones safaricom line. There also exists a whole host of privately run telemedicine schemes like Connect Med (mDaktari) by Access Afya, which aim to offer affordable convenient access to primary care.
Five years on and with the devolution of healthcare coupled with little or no change in primary healthcare delivery services especially in rural and marginalised areas, we would like to know of your experience of telemedicine and if it has truly revolutionised primary healthcare delivery for the rural poor and marginalised communities as envisioned. Have you heard of these schemes or even used any of them or any other form of telemedicine? If so, what has been your experience and what if anything can be improved upon?
Please let us know via the ‘your health matters’ page on the website.
Useful reading:
Nakweya,G(2015) Kenya launches telemedicine initiative for the poor- https://www.scidev.net/sub-saharan-africa/medicine/news/kenya-launches-telemedicine-initiative-poor.html
2. Wanyonyi,P(2015), Telemedicine is here ,but more needs to be done . Nairobi business monthly https://www.nairobibusinessmonthly.com/telemedicine-is-here-but-more-needs-to-be-done/
4. Kabia, J (2018), Technology expert says Kenya is the ‘promised land’ of telemedicine. Health Business- http://www.healthbusiness.co.ke/2015/technology-expert-says-kenya-is-the-promised-land-of-telemedicine/
Is patient feedback relevant and/or necessary?
Importance of feedback and how it can be used.
We all get some sort of feedback while going about our daily lives. It can be positive, critical, negative, unsolicited or at times asked for.
This also applies to institutions we interact with. We might give feedback whether asked for or not as pertaining to their services. Healthcare is big business and as a business, feedback from your service users in essential and should be incorporated into daily practice. Feedback is a great tool that can be used to evaluate how you are doing as an individual( useful for staff appraisals etc) or as a corporation ( improve or maintain high ranking, and increase revenue), and can be used to improve services or used to highlight strengths.
The National Institute for Health Research ( NIHR ) in the U.K has published an interesting piece of research looking at patient feedback and how it can be used to improve care. Please have a read below.:
https://content.nihr.ac.uk/nihrdc/themedreview-04327-PE/Patient-Feedback-WEB.pdf