Self-Swabbing Vs In-Person Smear Test: What's your choice?
Gynaecological cancers refer to the cancers that affect the female reproductive system such as the ovaries, uterus, cervix, fallopian tubes, vulva, and vagina. According to Eve Appeal, which is the U.K’s Gynaecological Cancer Research Charity, that raises awareness and funds research into the five common gynaecological cancers: Womb, Ovarian, Cervical, Vulval and Vaginal, there are over twenty two thousand new cases of gynaecological cancer every year in the U.K. Symptoms of gynaecological cancers may include pelvic and abdominal pain, bloating, abnormal vaginal bleeding, and changes in bowel habits. Early detection and treatment are crucial for the successful management of these cancers. Regular gynaecological screenings, including Pap tests and pelvic exams, can help detect these cancers in the early stages. Understanding the risks and symptoms associated with gynaecological cancers is important for all women to help prevent and manage these potentially life-threatening conditions.
Cervical screening, also known as a smear test, is an important preventative healthcare measure for women. The test involves taking a small sample of cells from the cervix to check for any abnormalities that could lead to cervical cancer. It is recommended that women aged between 25 and 64 years old should have a cervical screening every three to five years, depending on previous results, and those who are living with HIV should have one every year. Early detection of abnormal cells can lead to prompt treatment and a higher chance of successful outcomes. It is a simple and relatively quick procedure that can help to save lives, so it is important for all eligible women to participate in regular cervical screening.
Women in a park
There are two main types of cervical screening tests: the Pap test and the HPV test. The traditional Pap test involves collecting cells from the cervix and examining them under a microscope for any abnormal cells. This test can detect early signs of cervical cancer and is typically recommended for women aged 21 to 65. On the other hand, the HPV test checks for the presence of the human papillomavirus (HPV), which is the main cause of cervical cancer. This test can be done alone or in conjunction with a Pap test and is typically recommended for women aged 30 or older. It's important for women to discuss with their healthcare provider which type of screening is best for them and how often they should be screened.
Self swabbing tests have recently been introduced to allow women who would otherwise be uncomfortable with in-person tests or do not have time to attend in-person screening appointments. The self swabbing smear test is a much more convenient way to get checked for cervical cancer. Going for an in person smear test can be a daunting experience for some women. However, the self swabbing test can be done comfortably at home by following the instructions carefully. It also saves time and eliminates the need to visit a healthcare facility. On the other hand, an in person smear test is still necessary for some women, particularly those who may require additional medical attention or have difficulty performing the self swabbing test. Despite the slightly invasive nature of in person tests, they remain an essential part of women's health care, and they should never be ignored.
While i am all in favour of Self Swabbing for all the reasons listed above plus that it provides some sort of screening for those women who would have fallen through the cracks, i am still a firm believer in in-person smear tests because of the extra level of safety net it provides. Let me explain!
Woman sitting on couch
When i attend my smear test appointment ( which takes weeks of me psyching myself up), the nurse has a general conversation with me about how i am doing and if there have been any changes since my last smear test. Once i am lying down and in position and comfortable, she checks my vulva area for any changes, then feels for any swollen glands and once she is satisfied that everything looks healthy and alright, she inserts the speculum and continues with the smear test. Once all is done, i leave the appointment reassured that whilst i wait for my results, i am relaxed in the knowledge that my pelvic exam was otherwise normal and that i have no signs or symptoms of vulval cancer. But while in-person smear testing is my preferred choice of testing, i will leave you with the Pro and Cons of both, so that you can decide which one you would prefer, if not both.
Pros and Cons of Self-Swabbing Smear Test
Self-swabbing smear test is becoming more common as an alternative to the traditional method. There are pros and cons to consider when deciding whether to go for self-swabbing or not.
# Pros:
1. Less invasive - Self-swabbing test is less invasive because women do not require insertion of the speculum. This makes the procedure more comfortable for some women.
2. More privacy - Self-swabbing smear test allows women to perform the test in the privacy of their own homes. This enables women who find the traditional smear test embarrassing to have the test without feeling embarrassed.
3. Convenient - Women do not need to book an appointment or visit a clinic for a self-swabbing smear test. The self-swab can be done at home at a convenient time.
4. Cost-effective - Self-swabbing smear tests are usually cheaper than the traditional smear tests performed by medical professionals. This makes it a more affordable option for women who may not be able to afford the regular smear test fees.
# Cons:
1. Potential for inaccurate results - Self-swabbing may not be as accurate as the traditional smear test because the sample could be contaminated or insufficient,
Pros and Cons of In-person Smear Test
# Pros
Accuracy: In-person smear tests are generally more accurate than at-home tests.
Thoroughness: A healthcare professional can perform a more thorough exam during an in-person smear test.
Immediate Results: Depending on the facility, results can be available immediately after the test is performed.
Availability of Follow-up Care: If any abnormalities are detected, the healthcare professional can offer follow-up care or referrals for treatment.
Experienced Medical Professionals: The healthcare professional performing the test has undergone training and has experience in performing smear tests.
# Cons
Discomfort and Pain: For some individuals, smear tests can be uncomfortable or even painful.
Embarrassment or Shame: There may be cultural or personal barriers that make the test cumbersome or shameful to undergo.
Time and Effort: An in-person smear test requires scheduling an appointment and taking time out of one's day to travel to the facility.
So whichever method you choose, just remember that early detection saves lives and it is important to have your screening done when invited to have one.
How do you want to DIE?
Death, be it our own or a loved ones is something that causes a profound sense of loss to those that are close to us and can raise lots of questions and evoke emotions like guilt: How did they die? did they plan their death? Did we respect their wishes? How do i want my death to be?
As a society, and here i mean the British society, we tend to shy away from talking about death and dying.
We have compiled some information from two great Doctors about death and dying to get the conversation going and to make talking about death and dying less of a taboo but a part of normal life conversation.
Dr Kathryn Mannix is a Retired palliative care doctor. Writer: 'With the End in Mind', 'Listen.' Wants us to understanding dying more, fear it less, listen better.
Below is a powerful piece by her where she talks about dying and why we need to talk about death and dying.
Dr Linda Dykes also talks about the importance of having that conversation about CPR and how it is you want to die?
“CPR is not a treatment for #ordinarydying. Every instance of futile CPR - which is what will happen if nobody has sorted out the protection of a DNACPR for someone whose life is coming to an end - is a tragedy. Please, doctors, nurses, patients, families - #havetheconversation.”
Racial Profiling and Preconceived Notions in Healthcare in relation to Patient Care and Safety.
Racial profiling in hospitals is a patient safety issue.
Television programmes be they soaps or american medical shows, have always played a part in highlighting topical issues that are occurring in society in a more relatable way to the general public. We have seen EastEnders tackle issues around cancer, sexual consent and rape culture, schizophrenia, New Amsterdam and the opioid crisis, just to mention a few. Medical firsts have also been premiered in television medical shows and later we have been made aware of real life stories of those who have undergone these pioneering procedures.
The issue of race and its influence on healthcare provision and access is now coming to the forefront, especially after the Black Lives Matter protests and the healthcare disparities that have been laid bare by the Covid19 pandemic. This has come as no surprise to most BME patients and healthcare workers who have long known about these issues, raised concerns about them only to have nothing done to address them with business carrying on as usual.
The Good Doctor is an american television medical show, that in one of their recent episodes( season 4, episode 9), dealt with the issue of racial profiling in current medicine practice as well as forcing one of their resident doctors to take a hard look inwardly and confront their own preconceived notions. Claire, the doctor in question had been called to the emergency room to attend to a patient who happened to be a black woman who had experienced a cardiac event. Zara, the patient was on anti-hypertensive medication and was insistent that she was taking them as prescribed and had even brought them along with her, only in the confusion, she couldn't find which pocket she had placed them in. Claire on the other hand considered Zara ‘loud and messy’ and did not believe that she was compliant with taking her medication(which Zara did find eventually).Instead she used a pattern- processing technique that she had learnt in medical school which supported her case that ‘loud and messy’ black people always lied about their compliance and went ahead and administered an ACE inhibitor to try bring down Zara’s blood pressure which in turn led to complications with Zara needing open heart surgery as a result! Zara later learns of Claire’s assumptions based on racial profiling, requests that she is taken of her case and later confronts Claire , who feels afronted that she would be considered racist! You see, Claire was a black doctor, who had based her assumptions on her own experiences of being racially profiled and constantly having to prove herself to get to where she was and ‘loud and messy’ Zara was everything she was trying not to be so as to fit in a predominantly white environment. This was also the experience of a fellow non white doctor. Basically, they had to check their blackness at the door. How many times as a black nurse or patient have you been required to or felt the need to “check your blackness at the door” for you to get where you need to be or treatment. I know i have and this episode got me reflecting on instances during my work where racial profiling and or preconceived notions has been at play and where it has been framed as ‘the problem patient’ and my role if any in those scenarios.
Working on an acute medical ward, especially if it is a short stay one, you get to see familiar faces often in terms of patients and at times predictions can be made as to when they are likely to come back. These predictions could be based on certain trends illnesses take based on weather patterns and seasons and others are based on compliance and social issues. This is common amongst patients living with long term conditions, who more often than not have borne the brunt of cuts in services, speciality ward closures which in turn means they are in hospital more times than they would like.
Working on one such ward, we often had patients who had come in after a flare up of their conditions and subsequently admitted to the short stay unit. One such group of patients were those who suffered from sickle cell disease, a young demographic, who were trying to live their lives the best way they knew how. Somehow these patients had been labelled as problem patients, so much so that as soon as you walked through the door on your way to handover, you would be briefed on how many had been admitted or were on their way to the unit. One particular patient, got double the warnings and lookout calls from management. All this was because of pain management , what the doctors and nurses thought was best for the patients( little or no opiods) and what the patients rightly so argued was not working for them( lack of opiods or hostility towards them when opiods are requested). The scene as usual was set, the nurses and doctors caring for these patients already on the defensive and on the lookout, tensions palpable waiting for the so called problem patients. The patients on the other hand are also on the defensive and know that they have to fight again to get the pain relief and care that they deserved. This was a constant, ongoing scenario and we were more often than not so caught up in the battle of wits that we forgot to see the patient, the person behind the label. Yes we doled out care and medicines as prescribed, ticked the required boxes, freed up beds as fast as they were needed, often under very stressful and pressurised conditions not to mention short staffed. Care became automated, assembly line like.
Several studies have now shown that there is a great racial bias in pain assessment and management when it comes to black patients. Black patients, like these sickle cell patients are systematically under-treated for pain, especially when it comes to getting an opiod prescription. This was compounded by the fact that almost all speciality wards had been axed and closed across NHS trusts, where they would have received specialised care from a team that understood their disease process. Instead they were sent into a system that although provided care, it was care that was conditional and didn't meet their needs at best and was combatative at worst.
Years later, working within a specialist clinic, I had the chance to interact with one of the patients who had been labelled as doubly problematic when I was on the wards, from management to staff on the ground. The difference this time was that the management I worked under were aware and against the bad reputation this particular patient had been given all over the hospital and always made a point of mentioning the fact that, the patient was a young person, who was living their life despite their long term condition and the many complications( medically and socially) that came with it. In other words he made sure we saw the person behind the condition and focused on the person. He re-framed the equation from ‘problem patient’ to a person dealing with a ‘problem condition’. This re-framing made a whole world of difference. You saw the young person who throughout their life has had to live and learn to cope with their disease. They have had to advocate and mostly fight to get heard and get the care they deserve. Often they have been dismissed and inorder to prove their case have had to question and record each and every aspect of their care in the midst of being labelled ‘probelematic’. They were just trying to survive, live and not to be consumed nor defined by their illness, colour of their skin or their socio-economic status.
The system is not perfect, no system ever is but we can strive to make it fair. If we are aware of our own and others preconceived notions and challenge them instead of buying into them because it is easier and or helps us fit in, be part of the gang then we are one step closer to creating a fairer system, if not an almost perfect one.
Racism and Inherent Bias in Health: A Patient Safety Issue? Navigating healthcare while Black: Part 2
Snap shot of racism issues raised in the last few weeks.
Growing up, going to hospital was a very serious affair. It often meant that one was very sick or that something was very wrong. You would often get people going to visit relatives or friends to check on them because they heard they had gone to hospital. I have often joked that we Africans only seek medical help or go to hospital when we are dying ie when things are serious! Other times we relied on herbal medicines and remedies or over the counter medication and just got on with life. I had not realised that this ideology was deeply rooted in myself, why go to hospital when a paracetamol here, an ibuprofen there, a little Vix/Rob could help ease the pain, plus there are more sick people in the world and so long as the pain was bearable, life went on. In fact I took pride in the fact that i was not a frequent visitor to the GP and surely that alone must have earned me brownie points and that if I finally came in for a consult they would look at my records and see that I had not been in to see them for near on 11 years and that for me to have come in, means things were serious- the dying African analogy thing! I mean my work sickness records matched my not visiting GP records, if that earned you brownie points at work surely it applied to my GP as well? How deluded i was! But before i explain my delusion and crash to earth moment, i need to highlight another issue that in my opinion is a huge determinant in the quality of healthcare we receive as Black and marginalised communities. These are my observations and experiences through the years and by sharing them i hope i start a conversation where we as individuals can look within ourselves and check our biases and maybe we can understand that sometimes the system is stacked against certain individuals making them invisible and that by the time they become visible, it is not because they were neglectful with their own health or that they did not try hard enough, it just got too exhausting trying to get the help they needed and finally they gave up and that those racist views and practices at the top that we constantly deal with at work, school, in life, have a knock on effect that then affects society as a whole.
Before moving to Birmingham in 2005, we lived i a quiet mainly white neighbourhood within a small town. The GP practice was a small family practice with a handful of doctors and a lovely pair of receptionists who even while talking to you in person or over the phone, getting more information before sign posting you to the right service, did it with kindness and patience more often than not. You always felt welcome, never rushed and every concern was dealt with in house or via referral. Slowly the town started to grow, the independent shops were knocked down, a huge Tesco was built and new apartment blocks started springing up and the GP surgery got busy. The town was growing and changing, a natural progress. The area we moved to in Birmingham and indeed Birmingham as whole was much quieter and laid back than London, the traffic was almost none existent, it seemed like by 12 midday, especially on weekends everything just died, it was way to quiet but on the up side we could afford a bigger house with garden and the neighbours seemed nice. We registered with the local GP surgery, which was almost like the one we had left in London, despite the incident with the practice nurse or occasional gaffe by one of the GP partners who upon seeing the children during a consult said: “ what fat children! Very different from the ones I have been seeing in South Africa this last month” ( She had just come from a volunteering programme in South Africa), overall you felt heard and more importantly you saw your named doctor and the continuity of care was there. The receptionists were kind and you could walk in to make an appointment . The streets were clean, we knew the local street cleaner and would stop for a chat once in awhile. A year in we started to notice for sale signs cropping up, the white folk in the neighbourhood were moving out. Not long after, the local street cleaner left, said he was retiring and for a week a two we had a replacement and then nothing and they would be cleaned as and when. The area started to look neglected and derelict. Various take away shops started to crop up. Our corner part of town was changing and growing and not for the better it looked and the GP surgery was not spared this growth. We were getting an upgrade, a bigger and better service, it looked like but looks can be deceiving and not all change is good, especially when an area is changing and becoming more derelict and unkempt and phrases like ‘ deprived area ‘ start being banded around. When an area is now mostly inhabited by marginalised communities and it looks like the local council has all but given up and services such as litter picking, rubbish collection, housing and the community surroundings as a whole take a back foot, you start to realise how all this connects to healthcare provision, schooling, policing and life in general. A two tier system comes into play.
A year after my life altering surgery, i was back at work navigating the pitfall that is the extreme sport of nursing while black, especially in a new town, environment and work culture and all the changes going on withing the neighbourhood largely went unnoticed or took awhile to notice as most of my time was spent at work and the only time i went to the GP surgery was to take the children for their immunisations etc. I had been told at my hospital outpatient follow up after the surgery that i would experience some lower abdominal pain which was normal due to scaring and so i managed my pain when it became unbearable by taking paracetamol and ibuprofen and occasionally buscopan. My local pharmacy was great and between myself and the pharmacist we always managed to puzzle stuff out which meant i was helping the GP service as well as the hospital service by not using up time that can be used by more urgent cases. Years went on and the pain slowly got worse but i put it down to scaring and work/ family pressures. More and more people were coming into hospital and complaining about their GP’s and access to services, from rude receptionists, seeing different doctors if you were lucky to be granted an audience and no continuity of care, it was easier to come into A&E. One chap had been to his GP ( one of those mega practices) several times complaining of chest and joint pains and each time his was given pain killers, then stronger ones which were eventually on repeat prescription! After a year of frustration and increasing pain and breathlessness he turned up in A&E and was diagnosed with TB. Another elderly chap had to go into A&E at the request of his GP’s receptionist at the frustration of the A&E doctors. His old GP had retired ( White Exodus) and the surgery had been taken over by another GP ( South Asian ) who only operated on a Thursday and worked the other days at his brothers practice in Solihull. This meant that his patients could only book appointments to see him on the Thursdays otherwise if they fell sick outside of that given day, then A&E was their only choice! He finally had to change GP’s to a bigger practice, when it took almost 4 months to fix a medication error with his diabetic medication, where he was previously on a combined tablet of Metformin 850mg/ pioglitazone 15mg but later changed to standalone tablets but with Pioglitazone at 30mg, when this error was later highlighted to the surgery( taking months to sort out) , the only explanation was that the standalone tablets were cheaper than the combined tablets! No recognition of the drug error/ potential harm caused to patient nor an apology. This is what care in a so called ‘deprived’ area had come down to!
After more than 11 years since my major surgery and managing the related pain on my own, it got to a point where the pain was massively affecting my quality of life. So i decided to seek the services of my GP to help find out why the pain was getting worse and also why it was mainly on the left side and not the right where the Fallopian tube had been taken off, also why i was needing to empty my bladder more often. My GP practice had under gone a huge change and had become one of those major practices with around 8-10 doctors. It was a mission getting an appointment and i was informed that i would see a duty doctor as opposed to my named GP as that would take weeks of waiting. So i turned up for my appointment with my husband ( he was not letting me go to hospital alone ever , since i almost never came back last time he did) , the doctor asked why wanted to see him, i told him i had given all that history to the receptionist but i could tell him again, so went to explain why i was there to his completely disinterested self. He then asked what is it i wanted him to do? and that i had been dealing with it for 11 years, so what did i expect him to do? I was stunned into silence, i tried to explain that yes i had been dealing with the pain for that long but i had come in for help because it was getting worse and affecting my quality of life and my work as well and that something didn’t feel right and that if he looked at my records he would see that i was not a frequent visitor to the surgery and that the fact that i had come in meant that i was not coping and needed help. He casually googled the medical term for ovulation pain, then proceeded to tell me that i was suffering from that and that i should would write me a prescription for Ibuprofen which i should try and that would sort out my pain and that i can not expect him to help me when i have no records and do not seek help and that if i need help i should fight for it and bang the door more and then i would be taken seriously as they would then wonder why i was frequenting the surgery and was not getting help/relief from interventions prescribed and so would take matters further. in other words, i had to be a problem patient to be taken seriously! I was gobsmacked and just sat there starring and not believing what i was hearing. I could see that if i stayed and continued arguing my point the situation would escalate into something serious, so we left. I don’t know who was more livid between myself and my husband.
I could tell you how after weeks of banging on proverbial doors I finally got an ultrasound and MRI scan, which showed fibroid growth and bulging disks, further banging led to useless misogynistic gynaecological referral and a most eye opening Orthopaedic appointment where I was being warned to look out for signs of Cauda Equina and to get myself a female gynaecologist. At this point I was just tired 😫. Not that the story ends there nor does my experience of bad healthcare even after changing Gp's ( still same area with super surgery ) and i’m sure mine is not the only story of struggle in getting proper healthcare as a black person not to mention as a woman ( indeed the black practice nurse at my new surgery was leaving due to racism at the surgery! Not to mention that a serious drug error almost occurred because my records had zilch on them, no one had bothered to populate my online GP records! Being a nurse saved the day.)
Historical and all through colonialism with attitudes that still extend to this day, Black people have always been at the bottom of any hierarchical structure, our value and worth was and is still considered below that of the Whites and South Asian and these biases exist in everyday lived lives of Black People no matter your standing in life. How many black Owned and led GP services are out there? I am yet to see a black doctor at a gp surgery! Maybe if there were it would at least be a start in evening out the playing field of healthcare navigation for black patients? Just a thought. All I know is that i’m tired of constantly fighting to live while Black, be at work, I'm school/University, access to healthcare not just bare minimum healthcare and tired of being blamed as a whole for health outcomes while the system is verily rigged and stacked to the rafters against any positive outcomes.
Meanwhile, when you see me at the hospital looking alot worse for wear with conditions that could have been treated had they been caught earlier, please don’t fall into that judgmental trap of “ why are these people so neglectful with their health while it’s free” ! Try to listen and get their story, you maybe the only one who cares enough at that point!
Independent Patient Safety Organisations:
Plan4ZERO- Patient Safety Movement: https://patientsafetymovement.org/product/plan4zero-pin-magnet/
Patient Safety Learning Hub ( U.K based ) : https://www.patientsafetylearning.org/the-hub
Courtesy of the Lansing Injury Law News ( available on the Patient Safety Learning Hub.
Where do broken hearts go? A midnight reflection on mental health and mental health services within hospitals.
Patient in a hospital bed.
Everywhere you turn, you are reminded that we are living in unusual times, with words like “unprecedented” banded around often. We are also reminded of self care and mental well-being due to the effects of the pandemic and lock-down changing our way of lives for the foreseeable future if not forever- whats being called “the new normal”.
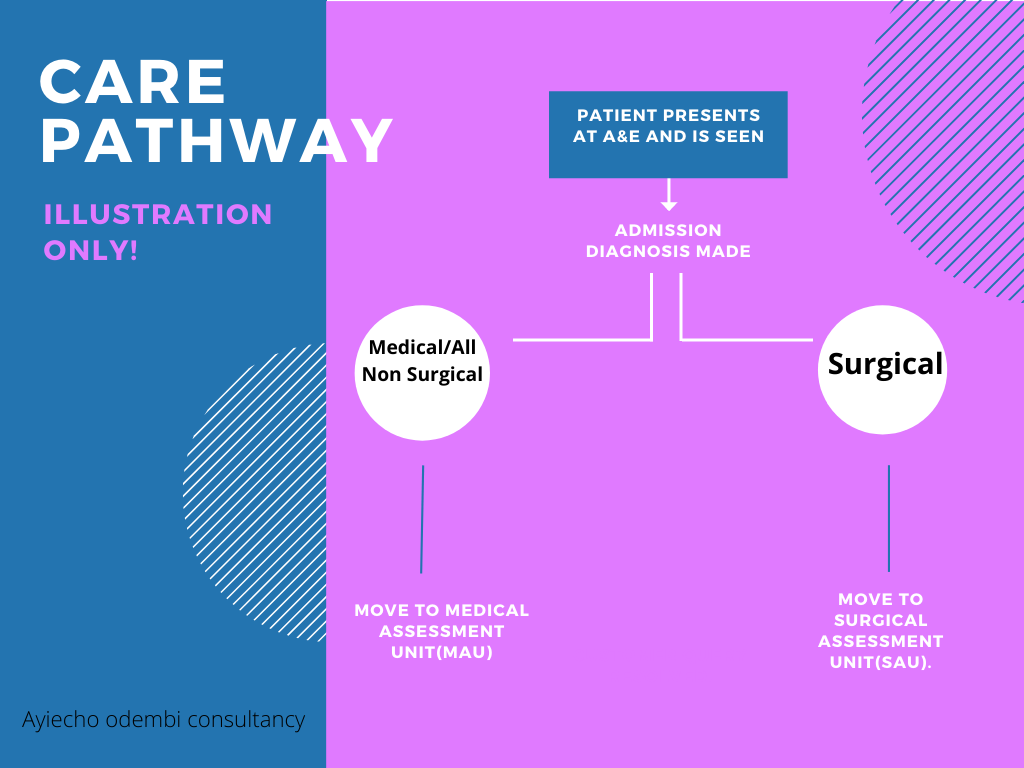
So there i was in the middle of the night, sleep having escaped me and Whitney Houston’s song ‘where do broken hearts go?’ playing over and over in my head, wondering where patients who presented with mental health problems went after coming into A&E? Or why , in my all my years in nursing, the only times i came across a mental health nurse was at university and when a psych consult was ordered on the unit/ward. Typically, when patients presented in A&E, and need admission, there are two routes normally followed- admission to the Medical assessment unit(MAU) or to the Surgical assessment unit(SAU). Most mental health patients end up in MAU or poisons unit( if admitted due to overdose and where such a unit is available and has empty beds).
Most of the time i have been involved in looking after a patient with mental health issues, it has been on an acute medical ward. This has been usually in the bays closest to the nurses patients reserved for patients who are acutely ill and need constant nursing supervision, which often involves bright lights, regular vital sign monitoring and other checks as per care plan with a hive of activity going on around due to the nature of varying acutely ill patients around. This got me wondering if an acute medical ward really is the right setting for someone going through a mental health crisis, given that they are being looked after by nurses, not mental health nurses, who yes might be doing a brilliant job and are good at what they do but are not aware of triggers or care pathways for someone going through a mental health crisis as a trained mental health nurse would with the patient in the right setting.
With a little help………
According to Mind¹, a leading mental health charity, mental health problems are common in England with 1 in 4 people experiencing some sort of mental health problem each year and 1 in 6 reporting having experienced a common mental health problem like anxiety or depression in any given week.
A study by The Nuffield Trust² looking at hospital use by people with mental health illness, makes for an interesting and sober reading and highlights a number of key points that need addressing. With almost every NHS hospital trust having a Medical assessment unit or a Surgical one, maybe it is time there was also a Mental health assessment unit where those coming into hospital with a mental health illness can get the care they deserve, looked after by trained mental health staff under conducive conditions designed with them in mind. I would certainly welcome a unit like that, where me and my fellow healthcare workers can pop into just for a chat or to make sense of life and all its challenges especially after a hard and emotionally draining day at work given the pressures we are constantly under with the added effect that this pandemic adds to it and i would be happy to know that mental health just like physical health, matters and that those going through any sort of mental health illness can come into hospital knowing that they have a dedicated area that’s ready to to help them in anyway possible.
Dr. Chisholm - the first Director-General of the World Health Organisation (WHO)